Spinal tumor
Tumor - spinal cord
A spinal tumor is a growth of cells (mass) in or around the spinal cord.
Causes
Any type of tumor may occur in the spine, including primary and secondary tumors.
Primary tumors: most of these tumors are benign and slow growing.
- Astrocytoma: a tumor of the supporting cells inside the spinal cord
- Meningioma: tumor of the tissue that covers the spinal cord
- Schwannoma: a tumor of the cells surrounding the nerve fibers
- Ependymoma: a tumor of the cells that line the cavities of the brain
- Lipoma: a tumor of the fat cells
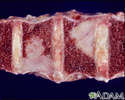
Secondary tumors or metastasis: these tumors are cancer cells coming from other areas of the body.
- Prostate, lung, and breast cancers
- Leukemia: a blood cancer that starts in the white cells in the bone marrow
- Lymphoma: a cancer of the lymph tissue
- Myeloma: a blood cancer that starts in the plasma cells of the bone marrow
The cause of primary spinal tumors is unknown. Some primary spinal tumors occur with certain inherited gene mutations.
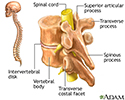
Spinal tumors can be located:
- Inside the spinal cord (intramedullary)
- In the membranes (meninges) covering the spinal cord (extramedullary - intradural)
- Between the meninges and bones of the spine (extradural)
- In the spine bones (vertebrae)
As it grows, the tumor can affect the:
- Blood vessels
- Bones of the spine
- Meninges
- Nerve roots
- Spinal cord cells
The tumor may press on the spinal cord or nerve roots, causing damage. With time, the damage may become permanent.
Symptoms
The symptoms depend on the location, type of tumor, and your general health. Secondary tumors that have spread to the spine from another site (metastatic tumors) often progress quickly. Primary tumors often progress slowly over weeks to years.
Symptoms may include:
- Abnormal sensations or loss of sensation, especially in the legs
- Back pain that gets worse over time, is often in the middle or lower back, is usually severe and not relieved by pain medicine, gets worse when lying down or straining (such as during a cough or sneeze), and may extend to the hips or legs
- Loss of bowel control, bladder leakage
- Muscle contractions, twitches, or spasms (fasciculations)
- Muscle weakness (decreased muscle strength) in the legs that causes falls, makes walking difficult, and may get worse (progressive) and lead to paralysis
Exams and Tests
A nervous system (neurological) examination may help pinpoint the location of the tumor. The health care provider may also find the following during an exam:
- Abnormal reflexes
- Increased muscle tone
- Loss of pain and temperature sensation
- Muscle weakness
- Tenderness in the spine
These tests may confirm spinal tumor:
- Spinal CT
- Spine MRI
- Spine x-ray
- Cerebrospinal fluid (CSF) examination
- Myelogram (x-ray of the spinal canal that contains the spinal cord)
- PET scan
Treatment
The goal of treatment is to reduce or prevent nerve damage caused by pressure on (compression of) the spinal cord and ensure that you can walk.
Treatment should be given quickly. The more quickly symptoms develop, the sooner treatment is needed to prevent permanent injury. Any new or unexplained back pain in a patient with cancer should be thoroughly investigated.
Treatments include:
- Corticosteroids (dexamethasone) may be given to reduce inflammation and swelling around the spinal cord.
- Emergency surgery may be needed to relieve compression on the spinal cord. Some tumors can be completely removed. In other cases, part of the tumor may be removed to relieve pressure on the spinal cord.
- Radiation therapy may be used with, or instead of, surgery.
- Chemotherapy has not been proven effective against most primary spinal tumors, but it may be recommended in some cases, depending on the type of tumor.
- Physical therapy may be needed to improve muscle strength and the ability to function independently.
Outlook (Prognosis)
The outcome varies depending on the tumor. Early diagnosis and treatment usually leads to a better outcome.
Nerve damage often continues, even after surgery. Although some amount of permanent disability is likely, early treatment may delay major disability and death.
When to Contact a Medical Professional
Contact your provider if you have a history of cancer and develop severe back pain that is sudden or gets worse.
Go to the emergency room or call 911 or the local emergency number if you develop new symptoms, or your symptoms get worse during the treatment of a spinal tumor.
References
DeAngelis LM. Tumors of the central nervous system. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 180.
Jakubovic R, Ruschin M, Tseng CL, Pejovic-Milic A, Sahgal A, Yang VXD. Surgical resection with radiation treatment planning of spinal tumors. Neurosurgery. 2019;84(6):1242-1250. PMID: 29796646 pubmed.ncbi.nlm.nih.gov/29796646/.
Moron FE, Delumpa A, Szklaruk J. Spinal tumors. In: Haaga JR, Boll DT, eds. CT and MRI of the Whole Body. 6th ed. Philadelphia, PA: Elsevier; 2017:chap 30.
Niglas M, Tseng C-L, Dea N, Chang E, Lo S, Sahgal A. Spinal cord compression. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 54.
Soliman H, Fridely J, Oyelese A, Gokaslan ZL. Management of spinal metastatic tumors. In: Ellenbogen RG, Sekhar LN, Kitchen ND, da Silva Hb, eds. Principles of Neurological Surgery. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 32.
Review Date: 8/15/2022
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.