Membranous nephropathy
Membranous glomerulonephritis; Membranous GN; Extramembranous glomerulonephritis; Glomerulonephritis - membranous; MGN
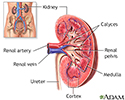
Membranous nephropathy is a kidney disorder that leads to changes and inflammation of the structures inside the kidney that help filter wastes and fluids. The inflammation may lead to problems with kidney function.
Causes
Membranous nephropathy is caused by the thickening of a part of the glomerular basement membrane. The glomerular basement membrane is a part of the kidneys that helps filter waste and extra fluid from the blood. The exact reason for this thickening is not known.
The thickened glomerular membrane does not work normally. As a result, large amounts of protein are lost in the urine.
This condition is one of the most common causes of nephrotic syndrome. This is a group of symptoms that include protein in the urine, low blood protein level, high cholesterol levels, high triglyceride levels, and swelling. Membranous nephropathy may be a primary kidney disease, or it may be associated with other conditions.
The following increase your risk for this condition:
- Cancers, especially lung and colon cancer
- Exposure to toxins, including gold and mercury
- Infections, including hepatitis B, malaria, syphilis, and endocarditis
- Medicines, including penicillamine, trimethadione, and skin-lightening creams
- Systemic lupus erythematosus, rheumatoid arthritis, Graves disease, and other autoimmune disorders
The disorder occurs at any age, but is more common after age 40.
Symptoms
Symptoms often begin slowly over time, and may include:
- Edema (swelling) in any area of the body
- Fatigue
- Foamy appearance of urine (due to large amounts of protein)
- Poor appetite
- Urination, excessive at night
- Weight gain
Exams and Tests
A physical exam may show swelling (edema).
A urinalysis may reveal a large amount of protein in the urine. There may also be some blood in the urine. The glomerular filtration rate (the "speed" at which the kidneys cleanse the blood) is often nearly normal.
Other tests may be done to see how well the kidneys are working and how the body is adapting to the kidney problem. These include:
- Albumin - blood and urine
- Blood urea nitrogen (BUN)
- Creatinine - blood
- Creatinine clearance
- Lipid panel
- Protein - blood and urine
A kidney biopsy confirms the diagnosis.
The following tests can help determine the cause of membranous nephropathy:
- Antinuclear antibodies test
- Anti-double-strand DNA, if the antinuclear antibodies test is positive
- Blood tests to check for hepatitis B, hepatitis C, and syphilis
- Complement levels
- Cryoglobulin test
Treatment
The goal of treatment is to reduce symptoms and slow the progression of the disease.
Controlling blood pressure is the most important way to delay kidney damage. The goal is to keep blood pressure at or below 130/80 mm Hg.
High blood cholesterol and triglyceride levels should be treated to reduce the risk for atherosclerosis. However, a low-fat, low-cholesterol diet is often not as helpful for people with membranous nephropathy.
Medicines used to treat membranous nephropathy include:
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) to lower blood pressure
- Corticosteroids and other medicines that suppress the immune system
- Medicines (most often statins) to reduce cholesterol and triglyceride levels
- Water pills (diuretics) to reduce swelling
- Blood thinners to reduce the risk for blood clots in the lungs and legs
Low-protein diets may be helpful. A moderate-protein diet (1 gram [gm] of protein per kilogram [kg] of body weight per day) may be suggested.
Vitamin D may need to be replaced if nephrotic syndrome is long-term (chronic) and does not respond to therapy.
This disease increases the risk for blood clots in the lungs and legs. Blood thinners may be prescribed to prevent these complications.
Outlook (Prognosis)
The outlook varies, depending on the amount of protein loss. There may be symptom-free periods and occasional flare-ups. Sometimes, the condition goes away, with or without therapy.
Most people with this disease will have kidney damage and some people will develop end-stage renal disease.
Possible Complications
Complications that may result from this disease include:
- Chronic renal failure
- Deep venous thrombosis
- End-stage renal disease
- Nephrotic syndrome
- Pulmonary embolism
- Renal vein thrombosis
When to Contact a Medical Professional
Contact your health care provider if:
- You have symptoms of membranous nephropathy
- Your symptoms get worse or don't go away
- You develop new symptoms
- You have decreased urine output
Prevention
Quickly treating disorders and avoiding substances that can cause membranous nephropathy may reduce your risk.
References
Radhakrishnan J, Appel GB. Glomerular disorders and nephrotic syndromes. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 113.
Saha MK, Pendergraft WF, Jennette JC, Falk RJ. Primary glomerular disease. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 31.
Salant DJ, Cattran DC. Membranous nephropathy. In: Feehally J, Floege J, Tonelli M, Johnson RJ, eds. Comprehensive Clinical Nephrology. 6th ed. Philadelphia, PA: Elsevier; 2019:chap 20.
Review Date: 7/27/2021
Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.