Malaria
Quartan malaria; Falciparum malaria; Biduoterian fever; Blackwater fever; Tertian malaria; Plasmodium
Malaria is a parasitic disease that involves high fevers, shaking chills, flu-like symptoms, and anemia.
Causes
Malaria is caused by a parasite. It is passed to humans by the bite of infected anopheles mosquitoes. After infection, the parasites (called sporozoites) travel through the bloodstream to the liver. There, they mature and release another form of parasites, called merozoites. The parasites enter the bloodstream and infect red blood cells.
The parasites multiply inside the red blood cells. The cells then break open within 48 to 72 hours and infect more red blood cells. The first symptoms usually occur 10 days to 4 weeks after infection, though they can appear as early as 8 days or as long as a year after infection. The symptoms occur in cycles of 48 to 72 hours.
Most symptoms are caused by:
- The release of merozoites into the bloodstream
- Anemia resulting from the destruction of the red blood cells
- Large amounts of free hemoglobin being released into circulation after red blood cells break open, which can damage other organs such as the kidneys
Malaria can also be transmitted from a mother to her unborn baby (congenitally) and by blood transfusions. Malaria can be carried by mosquitoes in temperate climates, but the parasite disappears over the winter.
The disease is a major health problem in much of the tropics and subtropics. The Centers for Disease Control and Prevention estimates that there are 300 to 500 million cases of malaria each year. More than 1 million people die of it. Malaria is a major disease hazard for travelers to warm climates.
In some areas of the world, mosquitoes that carry malaria have developed resistance to insecticides. In addition, the parasites have developed resistance to some antibiotics. These conditions have made it hard to control both the rate of infection and spread of this disease.
Symptoms
Symptoms include:
- Anemia (condition in which the body doesn't have enough healthy red blood cells)
- Bloody stools
- Chills, fever, sweating
- Coma
- Convulsions
- Headache
- Jaundice
- Muscle pain
- Nausea and vomiting
Exams and Tests
During a physical examination, the health care provider may find an enlarged liver or enlarged spleen.
Tests that are done include:
- Rapid diagnostic tests, which are becoming more common because they are easier to use and require less training by laboratory technicians
- Malaria blood smears taken at 6 to 12 hour intervals to confirm the diagnosis
- A complete blood count (CBC) will identify anemia if it is present
Treatment
Malaria, especially falciparum malaria, is a medical emergency that requires a hospital stay. Chloroquine is often used as an anti-malarial medicine. But chloroquine-resistant infections are common in some parts of the world.
Possible treatments for chloroquine-resistant infections include:
- Artemisinin derivative combinations, including artemether and lumefantrine
- Atovaquone-proguanil
- Quinine-based regimen, in combination with doxycycline or clindamycin
- Mefloquine, in combination with artesunate or doxycycline
The choice of drug depends, in part, on where you got the infection.
Medical care, including fluids through a vein (IV) and other drugs and breathing (respiratory) support may be needed.
Outlook (Prognosis)
Outcome is expected to be good in most cases of malaria with treatment, but poor in falciparum infection with complications.
Possible Complications
Health problems that may result from malaria include:
- Brain infection (cerebritis)
- Destruction of blood cells (hemolytic anemia)
- Kidney failure
- Liver failure
- Meningitis
- Respiratory failure from fluid in the lungs (pulmonary edema)
- Rupture of the spleen leading to massive internal bleeding (hemorrhage)
When to Contact a Medical Professional
Contact your health care provider if you develop fever and headache after visiting any foreign country.
Prevention
Most people who live in areas where malaria is common have developed some immunity to the disease. Visitors will not have immunity and should take preventive medicines.
It is important to see your health care provider well before your trip. This is because treatment may need to begin as long as 2 weeks before travel to the area, and continue for a month after you leave the area. Most travelers from the United States who contract malaria fail to take the right precautions.
The types of anti-malarial drugs prescribed depend on the area you visit. Travelers to South America, Africa, the Indian subcontinent, Asia, and the South Pacific should take one of the following drugs:
- Mefloquine
- Doxycycline
- Chloroquine
- Hydroxychloroquine
- Atovaquone-proguanil
Even pregnant women should consider taking preventive drugs because the risk to the fetus from the drug is less than the risk of catching this infection.
Chloroquine has been the drug of choice for protecting against malaria. But because of resistance, it is now only suggested for use in areas where Plasmodium vivax, P oval, and P malariae are present.
Falciparum malaria is becoming increasingly resistant to anti-malarial medications. Recommended drugs include mefloquine, atovaquone/proguanil (Malarone), and doxycycline.
Prevent mosquito bites by:
- Wearing protective clothing over your arms and legs
- Using mosquito netting while sleeping
- Using insect repellent
For information on malaria and preventive medications, visit the CDC website: www.cdc.gov/malaria/travelers/index.html.
References
Ansong D, Seydel KB, Taylor TE. Malaria. In: Ryan ET, Hill DR, Solomon T, Aronson NE, Endy TP, eds. Hunter's Tropical Medicine and Emerging Infectious Diseases. 10th ed. Philadelphia, PA: Elsevier; 2020:chap 101.
Fairhurst RM, Wellems TE. Malaria (Plasmodium species). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 274.
Freedman DO. Protection of travelers. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 318.
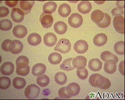
Malaria, microscopic view of cellular parasites - illustration
Malaria, microscopic view of cellular parasites
illustration
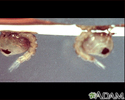
Mosquito, adult feeding on the skin - illustration
Mosquito, adult feeding on the skin
illustration
Mosquito, egg raft - illustration
Mosquito, egg raft
illustration
Mosquito, larvae - illustration
Mosquito, larvae
illustration
Mosquito, pupa - illustration
Mosquito, pupa
illustration
Malaria, microscopic view of cellular parasites - illustration
Malaria, microscopic view of cellular parasites
illustration
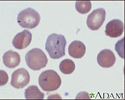
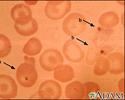
Malaria, photomicrograph of cellular parasites - illustration
Malaria, photomicrograph of cellular parasites
illustration
Malaria - illustration
Malaria
illustration
Digestive system organs - illustration
Digestive system organs
illustration
Malaria, microscopic view of cellular parasites - illustration
Malaria, microscopic view of cellular parasites
illustration
Mosquito, adult feeding on the skin - illustration
Mosquito, adult feeding on the skin
illustration
Mosquito, egg raft - illustration
Mosquito, egg raft
illustration
Mosquito, larvae - illustration
Mosquito, larvae
illustration
Mosquito, pupa - illustration
Mosquito, pupa
illustration
Malaria, microscopic view of cellular parasites - illustration
Malaria, microscopic view of cellular parasites
illustration
Malaria, photomicrograph of cellular parasites - illustration
Malaria, photomicrograph of cellular parasites
illustration
Malaria - illustration
Malaria
illustration
Digestive system organs - illustration
Digestive system organs
illustration
Review Date: 6/20/2021
Reviewed By: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.