Tetralogy of Fallot
Tet; TOF; Congenital heart defect - tetralogy; Cyanotic heart disease - tetralogy; Birth defect - tetralogy
Tetralogy of Fallot is a type of congenital heart defect. Congenital means that it is present at birth.
Causes
Tetralogy of Fallot causes low oxygen levels in the blood. This leads to cyanosis (a bluish-purple color to the skin).
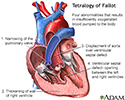
The classic form includes four defects of the heart and its major blood vessels:
- Ventricular septal defect (hole between the right and left ventricles)
- Narrowing of the pulmonary outflow tract (the valve and artery that connect the heart with the lungs)
- Overriding aorta (the artery that carries oxygen-rich blood to the body) that is shifted over the right ventricle and ventricular septal defect, instead of coming out only from the left ventricle
- Thickened wall of the right ventricle (right ventricular hypertrophy)
Tetralogy of Fallot is rare, but it is the most common form of cyanotic congenital heart disease. It occurs equally as often in males and females. People with tetralogy of Fallot are more likely to also have other congenital defects.
The cause of most congenital heart defects is unknown. Many factors seem to be involved.
Factors that increase the risk for this condition during pregnancy include:
- Alcoholism in the mother
- Diabetes
- Mother who is over 40 years old
- Poor nutrition during pregnancy
- Rubella or other viral illnesses during pregnancy
Children with tetralogy of Fallot are more likely to have chromosome disorders, such as Down syndrome, Alagille syndrome, and DiGeorge syndrome (a condition that causes heart defects, low calcium levels, and poor immune function).
Symptoms
Symptoms include:
- Blue color to the skin (cyanosis), which gets worse when the baby is upset
- Clubbing of fingers (skin or bone enlargement around the fingernails)
- Difficulty feeding (poor feeding habits)
- Failure to gain weight
- Passing out
- Poor development
- Squatting during episodes of cyanosis (which increases blood flow to the lungs)
Exams and Tests
A physical exam with a stethoscope almost always reveals a heart murmur.
Tests may include:
- Chest x-ray
- Complete blood count (CBC)
- Echocardiogram
- Electrocardiogram (ECG)
- MRI of the heart (generally after surgery)
- CT of the heart
Treatment
Surgery to repair tetralogy of Fallot is done when the infant is very young, typically before 6 months of age. Sometimes, more than one surgery is needed. When more than one surgery is used, the first surgery is done to help increase blood flow to the lungs.
Surgery to correct the problem may be done at a later time. Often only one corrective surgery is performed in the first few months of life. Corrective surgery is done to widen part of the narrowed pulmonary tract and close the ventricular septal defect with a patch.
Outlook (Prognosis)
Most cases can be corrected with surgery. Babies who have surgery usually do well. More than 90% survive to adulthood and live active, healthy, and productive lives. Without surgery, death often occurs by the time the person reaches age 20.
People who have excessive leakiness of the pulmonary valve after surgery (which is common) may need to have the valve replaced.
Regular follow-up with a cardiologist is strongly recommended.
Possible Complications
Complications may include:
- Delayed growth and development
- Irregular heart rhythms (arrhythmias)
- Seizures during periods when there is not enough oxygen
- Death from cardiac arrest, even after surgical repair
When to Contact a Medical Professional
Call your health care provider if new unexplained symptoms develop or the child is having an episode of cyanosis (blue skin).
If a child with tetralogy of Fallot becomes blue, immediately place the child on their side or back and put the knees up to the chest. Calm the child and seek medical attention right away.
Prevention
There is no known way to prevent the condition.
References
Bernstein D. Cyanotic congenital heart disease: evaluation of the critically ill neonate with cyanosis and respiratory distress. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, MBBS, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 456.
Valente AM, Dorfman AL, Babu-Narayan SV, Kreiger EV. Congenital heart disease in the adolescent and adult. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 82.
Well A, Fraser CD. Congenital heart disease. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 59.
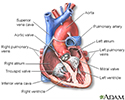
Heart - section through the middle - illustration
Heart - section through the middle
illustration
Tetralogy of Fallot - illustration
Tetralogy of Fallot
illustration
Cyanotic 'Tet spell' - illustration
Cyanotic 'Tet spell'
illustration
Review Date: 10/10/2021
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.