Health Library
Gastric bypass surgery
Bariatric surgery - gastric bypass; Roux-en-Y gastric bypass; Gastric bypass - Roux-en-Y; Weight-loss surgery - gastric bypass; Obesity surgery - gastric bypass
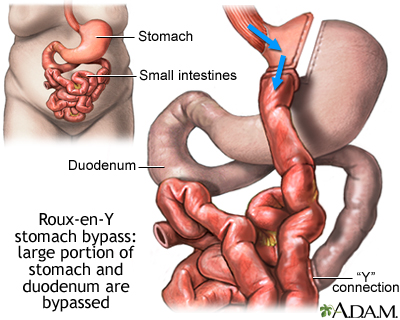
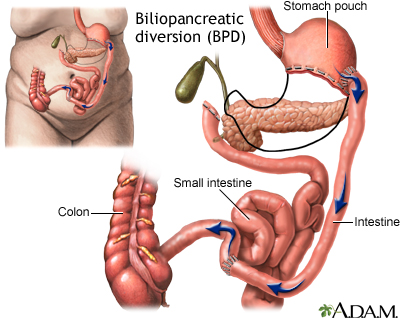
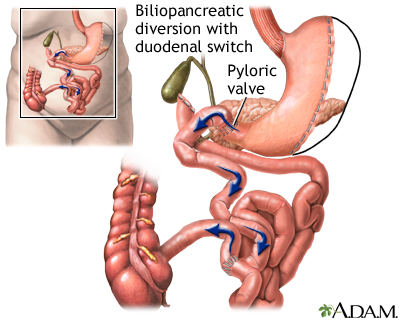
Gastric bypass is surgery that helps you lose weight by changing how your stomach and small intestine handle the food you eat.
After the surgery, your stomach will be smaller. You will feel full with less food.
The food you eat will no longer go into some parts of your stomach and small intestine that absorb food. Because of this, your body will not get all of the calories from the food you eat.
Images
I Would Like to Learn About:
Description
You will have general anesthesia before this surgery. You will be asleep and pain-free.
There are 2 steps during gastric bypass surgery:
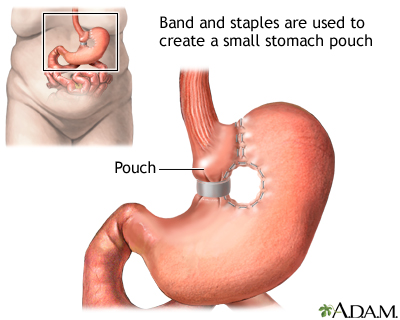
- The first step makes your stomach smaller. Your surgeon uses staples to divide your stomach into a small upper section and a larger bottom section. The top section of your stomach (called the pouch) is where the food you eat will go. The pouch is about the size of a walnut. It holds only about 1 ounce (oz) or 28 grams (g) of food. Because of this you will eat less and lose weight.
- The second step is the bypass. Your surgeon connects a part of your small intestine (the jejunum) to a small hole in your pouch. The food you eat will now travel from the pouch into this new opening and into your small intestine below where it would normally go, thus bypassing part of your small intestine. As a result, your body will absorb fewer calories.
Gastric bypass can be done in two ways. With open surgery, your surgeon makes a large surgical cut to open your belly. The bypass is done by working on your stomach, small intestine, and other organs.
Another way to do this surgery is to use a tiny camera, called a laparoscope. This camera is placed in your belly. The surgery is called laparoscopy. The scope allows the surgeon to see inside your belly.
In laparoscopy surgery:
- The surgeon makes 4 to 6 small cuts in your belly.
- The scope and instruments needed to perform the surgery are inserted through these cuts.
- The camera is connected to a video monitor in the operating room. This allows the surgeon to view inside your belly while doing the operation.
Advantages of laparoscopy over open surgery include:
- Shorter hospital stay and quicker recovery
- Less pain
- Smaller scars and a lower risk for getting a hernia or infection
This surgery takes about 2 to 4 hours.
Why the Procedure Is Performed
Weight-loss surgery (also called metabolic and bariatric surgery or MBS) may be an option if you have moderate to high-risk obesity and have not been able to lose enough weight through diet and exercise.
Health care providers often use the body mass index (BMI) and health conditions such as type 2 diabetes (diabetes that started in adulthood) and high blood pressure to determine which people are most likely to benefit from MBS.
Gastric bypass surgery is not a quick fix for obesity. It will greatly change your lifestyle. After this surgery, you must eat healthy foods, control portion sizes of what you eat, and exercise. If you do not follow these measures, you may have complications from the surgery and poor weight loss.
Be sure to discuss the benefits and risks with your surgeon.
This procedure may be recommended if you have:
- A BMI of 35 or more. Someone with a BMI of 35 or more is 80 or more pounds (36.3 kilograms) over their recommended weight. A normal BMI is 18.5 to 24.9. If you are a member of an Asian population, the BMI threshold for considering surgery is 27.5.
- A BMI of 30 to 34.9 (also called class 1 obesity) and a serious medical condition that might improve with weight loss. Some of these conditions are obstructive sleep apnea, type 2 diabetes, asthma, dyslipidemia, fatty liver disease, nonalcoholic steatohepatitis, and heart disease. If you are a member of an Asian population with one of these conditions, the BMI threshold for considering surgery is 25.
Risks
Gastric bypass is major surgery and it has many risks. Some of these risks are very serious. You should discuss these risks with your surgeon.
Risks of having anesthesia and surgery in general include:
- Allergic reactions to medicines
- Breathing problems
- Bleeding, blood clots, infection
- Heart problems
Risks of gastric bypass include:
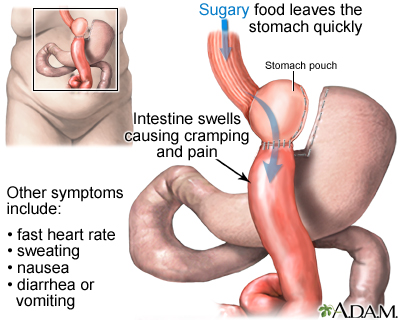
- Gastritis (inflamed stomach lining), heartburn, or stomach ulcers
- Injury to the stomach, intestines, or other organs during surgery
- Leaking from the line where parts of the stomach have been stapled together
- Poor nutrition
- Scarring inside your belly that could lead to a blockage in your bowel in the future
- Vomiting from eating more than your stomach pouch can hold
Before the Procedure
Your surgeon will ask you to have tests and visits with other health care providers before you have this surgery. Some of these are:
- A complete physical exam.
- Blood tests, ultrasound of your gallbladder, and other tests to make sure you are healthy enough to have surgery.
- Visits with your provider to make sure other medical problems you may have, such as diabetes, high blood pressure, and heart or lung problems, are under control.
- Nutritional counseling.
- Classes to help you learn what happens during the surgery, what you should expect afterward, and what risks or problems may occur afterward.
- You may want to visit with a counselor to make sure you are emotionally ready for this surgery. You must be able to make major changes in your lifestyle after surgery.
If you smoke, you should stop several weeks before surgery and not start smoking again after surgery. Smoking slows recovery and increases the risks for problems. Tell your provider if you need help quitting.
Tell your surgeon or nurse:
- If you are or might be pregnant
- What medicines, vitamins, herbs, and other supplements you are taking, even ones you bought without a prescription
During the week before your surgery:
- You may be asked to stop taking medicines that make it hard for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), warfarin (Coumadin), and others.
- Ask your surgeon which medicines you should still take on the day of your surgery.
- Prepare your home for after the surgery.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
Most people stay in the hospital for 1 to 4 days after surgery.
In the hospital:
- You will be asked to sit on the side of the bed and walk a little on the same day you have surgery.
- You may have a tube that goes through your nose into your stomach for 1 or 2 days. This tube helps drain fluids from your intestine.
- You may have a catheter in your bladder to remove urine.
- You will not be able to eat for the first 1 to 3 days. After that, you can have liquids and then pureed or soft foods.
- You may have a tube connected to the larger part of your stomach that was bypassed. The tube will come out of your side and will drain fluids.
- You will wear special stockings on your legs to help prevent blood clots from forming.
- You will receive shots of medicine to prevent blood clots.
- You will receive pain medicine. You will take pills for pain or receive pain medicine through an IV, a catheter that goes into your vein.
You will be able to go home when:
- You can eat liquid or pureed food without vomiting.
- You can move around without a lot of pain.
- You do not need pain medicine through an IV or given by shot.
Be sure to follow instructions for how to care for yourself at home.
Outlook (Prognosis)
Most people lose about 10 to 20 pounds (4.5 to 9 kilograms) a month in the first year after surgery. Weight loss will decrease over time. By sticking to your diet and exercise program from the beginning, you lose more weight.
You may lose one half or more of your extra weight in the first 2 years. You will lose weight quickly after surgery if you are still on a liquid or pureed diet.
Losing enough weight after surgery can improve many medical conditions, including:
- Asthma
- Arthritis
- Nonalcoholic fatty liver disease
- Gastroesophageal reflux disease (GERD)
- High blood pressure
- High cholesterol
- Obstructive sleep apnea
- Type 2 diabetes
Weighing less should also make it much easier for you to move around and do your everyday activities.
To lose weight and avoid complications from the procedure, you will need to follow the exercise and eating guidelines that your provider and dietitian have given you.
Related Information
Body mass indexObstructive sleep apnea - adults
Type 2 diabetes
Coronary heart disease
Obesity
Laparoscopic gastric banding
Bathroom safety for adults
Surgical wound care - open
Preventing falls
When you have nausea and vomiting
Gastric bypass surgery - discharge
Your diet after gastric bypass surgery
Laparoscopic gastric banding - discharge
After weight-loss surgery - what to ask your doctor
Before weight-loss surgery - what to ask your doctor
References
Eisenberg D, Shikora SA, Aarts E, et al. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): Indications for Metabolic and Bariatric Surgery. Surg Obes Relat Dis. 2022;18(12):1345-1356. PMID: 36280539 pubmed.ncbi.nlm.nih.gov/36280539/.
Richards WO, Khaitan L, Torquati A. Morbid obesity. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 48.
Schirmer B. Operations for morbid obesity. In: Yeo CJ, ed. Shackelford's Surgery of the Alimentary Tract. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 63.
Sullivan S, Edmundowicz SA, Morton JM. Surgical and endoscopic treatment of obesity. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 8.
BACK TO TOPReview Date: 8/22/2022
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 02/21/2023.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2023 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
