Health Library
Cellulitis
Skin infection - bacterial; Group A streptococcus - cellulitis; Staphylococcus - cellulitis
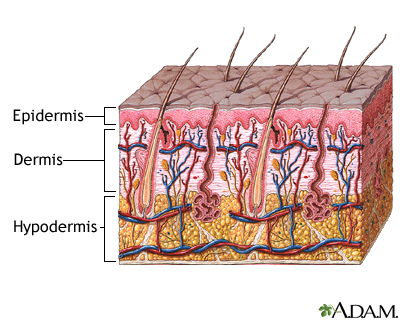
Cellulitis is a common skin infection caused by bacteria. It affects the middle layer of the skin (dermis) and the tissues below. Sometimes, muscle can be affected.
Images

I Would Like to Learn About:
Causes
Staphylococcus and streptococcus bacteria are the most common causes of cellulitis.
Normal skin has many types of bacteria living on it. When there is a break in the skin, these bacteria can cause a skin infection.
Risk factors for cellulitis include:
- Cracks or peeling skin between the toes
- History of peripheral vascular disease
- Injury or trauma with a break in the skin (skin wounds)
- Insect bites and stings, animal bites, or human bites
- Ulcers from certain diseases, including diabetes and vascular disease
- Use of corticosteroid medicines or other medicines that suppress the immune system
- Wound from a recent surgery
Symptoms
Symptoms of cellulitis include:
- Fever with chills and sweating
- Fatigue
- Pain or tenderness in the affected area
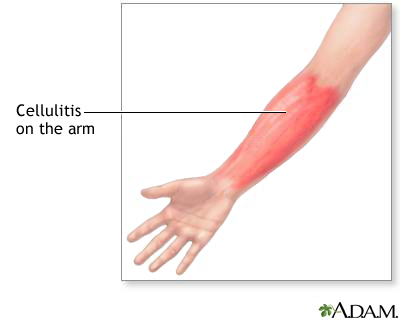
- Skin redness or inflammation that gets bigger as the infection spreads
- Skin sore or rash that starts suddenly, and grows quickly in the first 24 hours
- Tight, glossy, stretched appearance of the skin
- Warm skin in the area of redness
- Muscle aches and joint stiffness from swelling of the tissue over the joint
- Nausea and vomiting
Exams and Tests
The health care provider will perform a physical exam. This may reveal:
- Redness, warmth, tenderness, and swelling of the skin
- Possible drainage, if there is a buildup of pus (abscess) with the skin infection
- Swollen glands (lymph nodes) near the affected area
The provider may mark the edges of the redness with a pen, to see if the redness goes past the marked border over the next several days.
Tests that may be ordered include:
- Blood culture
- Complete blood count (CBC)
- Culture of any fluid or material inside the affected area
- A biopsy may be done if other conditions are suspected
Treatment
You will likely be prescribed antibiotics to be taken by mouth. You may be given pain medicine as well, if needed.
At home, raise the infected area higher than your heart to reduce swelling and speed up healing. Rest until your symptoms improve.
You may need to stay in a hospital if:
- You are very sick (for example, you have a very high temperature, blood pressure problems, or nausea and vomiting that does not go away)
- You have been on antibiotics and the infection is getting worse (spreading beyond the original pen marking)
- Your immune system is not working well (due to cancer, HIV)
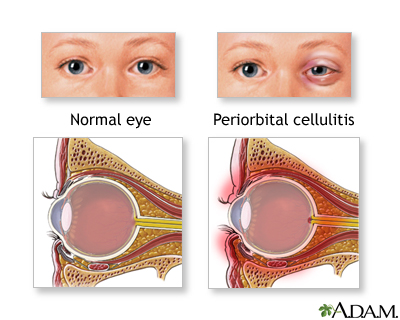
- You have an infection around your eyes
- You require antibiotics through a vein (IV)
Outlook (Prognosis)
Cellulitis usually goes away after taking antibiotics for 7 to 10 days. Longer treatment may be needed if cellulitis is more severe. This may occur if you have a chronic disease or your immune system is not working properly.
People with fungal infections of the feet may have cellulitis that keeps coming back, especially if you have diabetes. Cracks in the skin from the fungal infection allow the bacteria to get into the skin.
Possible Complications
The following may result if cellulitis isn't treated or treatment doesn't work:
- Blood infection (sepsis)
- Bone infection (osteomyelitis)
- Inflammation of the lymph vessels (lymphangitis)
- Inflammation of the heart (endocarditis)
- Infection of the membranes covering the brain and spinal cord (meningitis)
- Shock
- Tissue death (gangrene)
When to Contact a Medical Professional
Call your provider right away if:
- You have symptoms of cellulitis
- You are being treated for cellulitis and you develop new symptoms, such as persistent fever, drowsiness, lethargy, blistering over the cellulitis, or red streaks that spread
Prevention
Protect your skin by:
- Keeping your skin moist with lotions or ointments to prevent cracking
- Wearing shoes that fit well and provide enough room for your feet
- Learning how to trim your nails to avoid harming the skin around them
- Wearing appropriate protective equipment when participating in work or sports
Whenever you have a break in the skin:
- Clean the break carefully with soap and water. Apply petroleum jelly every day.
- Cover with a bandage and change it every day.
- Watch for redness, pain, drainage, or other signs of infection.
Related Information
AcuteErysipelas
Insect bites and stings
Peripheral artery disease - legs
Diabetes
Ulcers
Sepsis
Meningitis
Lymphadenitis
References
Dinulos JGH. Bacterial infections. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 9.
Heagerty AHM, Harper N. Cellulitis and erysipelas. In: Lebwohl MG, Heymann WR, Berth-Jones J, Coulson IH, eds. Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 5th ed. Philadelphia, PA: Elsevier; 2018:chap 40.
Pasternack MS, Swartz MN. Cellulitis, necrotizing fasciitis, and subcutaneous tissue infections. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 93.
BACK TO TOPReview Date: 4/14/2021
Reviewed By: Elika Hoss, MD, Senior Associate Consultant, Mayo Clinic, Scottsdale, AZ. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2022 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
