Health Library
Osteoporosis
Thin bones; Low bone density; Metabolic bone disease; Hip fracture - osteoporosis; Compression fracture - osteoporosis; Wrist fracture - osteoporosis
Osteoporosis is a disease in which bones become fragile and more likely to break (fracture).
Images
Animation


I Would Like to Learn About:
Causes
Osteoporosis is the most common type of bone disease.
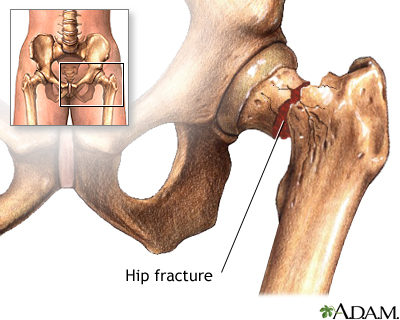
Osteoporosis increases the risk of breaking a bone. About one half of all women over the age of 50 will have a fracture of the hip, wrist, or vertebra (bones of the spine) during their lifetime. Spine fractures are the most common.
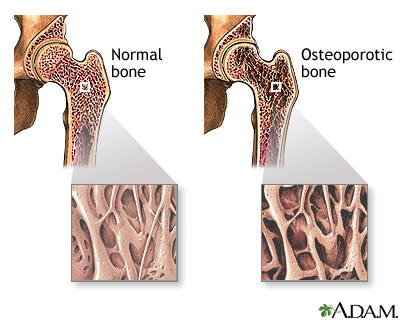
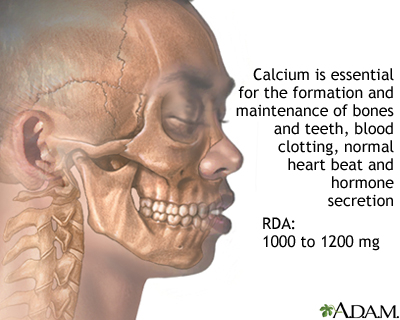
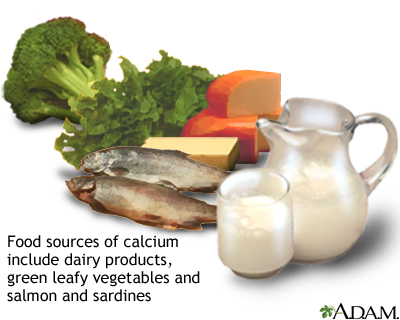
Your body needs the minerals calcium and phosphate to make and keep healthy bones.
- During your life, your body continues to both reabsorb old bone and create new bone.
- As long as your body has a good balance of new and old bone, your bones stay healthy and strong.
- Bone loss occurs when more old bone is reabsorbed than new bone is created.
Sometimes, bone loss occurs without any known cause. Other times, bone loss and thin bones run in families. In general, white, older women are the most likely to have bone loss.
Brittle, fragile bones can be caused by anything that makes your body destroy too much bone, or keeps your body from making enough new bone. As you age, your body may reabsorb calcium and phosphate from your bones instead of keeping these minerals in your bones. This makes your bones weaker.
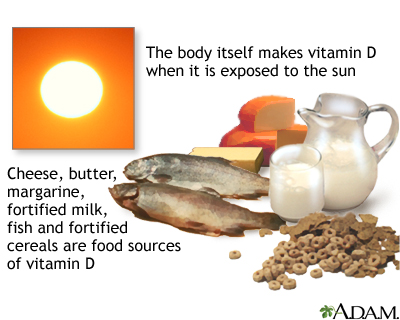
A major risk is not having enough calcium to build new bone tissue. It is important to eat/drink enough high-calcium foods. You also need vitamin D, because it helps your body absorb calcium. Your bones may become brittle and more likely to fracture if:
- If you do not eat enough food with calcium and vitamin D
- Your body does not absorb enough calcium from your food, such as after gastric bypass surgery
Other causes of bone loss include:
- A decrease in estrogen in women at the time of menopause and a decrease in testosterone in men as they age
- Being confined to a bed due to a prolonged illness (mostly affects bones in children)
- Having certain medical conditions that cause increased inflammation in the body
- Taking certain medicines, such as certain seizure medicines, hormone treatments for prostate or breast cancer, and steroid medicines taken for more than 3 months
Other risk factors include:
- Absence of menstrual periods for long periods of time
- A family history of osteoporosis
- Drinking a large amount of alcohol
- Low body weight
- Smoking
- Having an eating disorder, such as anorexia nervosa
- Certain ethnic groups have a higher rate of low bone mass
Symptoms
There are no symptoms in the early stages of osteoporosis. Many times, people will have a fracture before learning they have the disease.
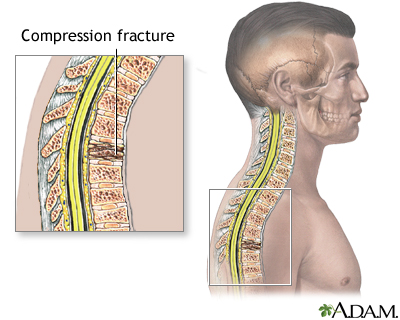
Fractures of the bones of the spine can cause pain almost anywhere in the spine. These are called compression fractures. They often occur without an injury. The pain occurs suddenly or slowly over time.
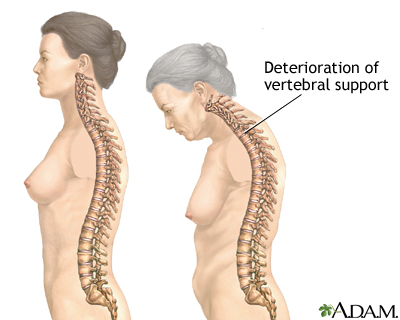
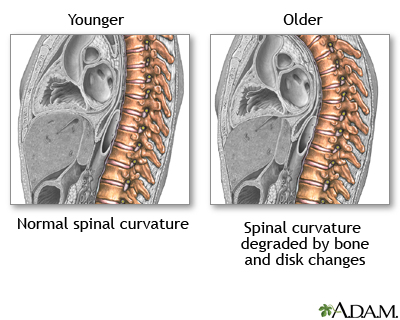
There can be a loss of height (as much as 6 inches or 15 centimeters) over time. A stooped posture or a condition called a dowager's hump may develop.
Exams and Tests
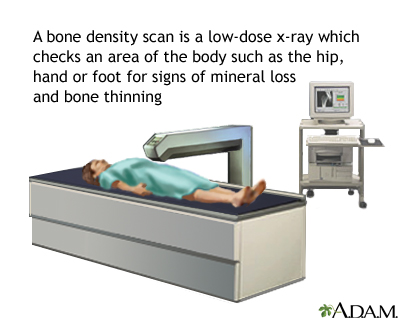
A DEXA scan is a low-radiation x-ray that measures the density of the minerals in your bones. Most often, it measures density in the spine and hip bones. Your health care provider uses this test to:
- Diagnose bone loss and osteoporosis.
- Predict your risk for future bone fractures.
- See how well osteoporosis medicine is working. (The DEXA is most often repeated every 2 years.)
A simple spine or hip x-ray may show fracture or collapse of the spinal bones. However, simple x-rays of other bones are not very accurate in predicting whether you are likely to have osteoporosis. A new low-radiation spine x-ray called a vertebral fracture assessment (VFA) is now often done with a DEXA to better identify fractures that do not have any symptoms.
You may need blood and urine tests if your provider thinks the cause of your osteoporosis is a medical condition, rather than the slow bone loss that occurs with aging.
DEXA scan results compare your bone mineral density with both a young adult who has no bone loss and with people your age and sex. This means that at age 80, almost one third of women with normal age-related bone loss would have osteoporosis, based on their DEXA scan results.
Treatment
Treatment for osteoporosis may involve:
- Making lifestyle changes, such as changing your diet and exercise routine
- Taking calcium and vitamin D supplements
- Using medicines
Medicines are used to strengthen bones when:
- Osteoporosis has been diagnosed by a bone density study, whether or not you have a fracture, and your fracture risk is high.
- You have had a bone fracture, and a bone density test shows that you have thin bones, but not osteoporosis.
Medicines used to treat osteoporosis include:
- Bisphosphonates -- the main drugs used to prevent and treat osteoporosis in postmenopausal women. They can be given by mouth or by IV.
- Denosumab -- lessens bone loss and increases bone density. Given by injection under the skin.
- Teriparatide or abaloparatide -- man-made forms of a hormone your body makes that increases bone density.
- Romosozumab -- a newer drug for more severe bone thinning.
- Estrogen receptor modulators.
- Calcitonin -- a man-made form of a hormone your body makes that increases bone density. Used mainly to treat the sudden pain from a spine fracture.
The length of time a woman needs to take these medicines depends on her level of risk. Recommendations include:
- Low fracture risk -- 5 years of oral medicine or 3 years of IV therapy
- High fracture risk -- 10 years of oral medicine or 6 years of IV therapy
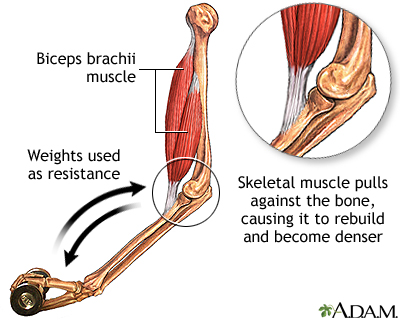
Exercise plays a key role in preserving bone density in older adults. Some of the exercises recommended to reduce your chance of a fracture include:
- Weight-bearing exercises, such as walking, jogging, playing tennis, or dancing for at least 30 minutes, three times per week.
- Free weights, weight machines, stretch bands
- Balance exercises, such as tai chi and yoga
- Rowing machines
Avoid any exercise that presents a risk of falling. Also, do not do high-impact exercises that can cause fractures in older adults.
Follow these guidelines for getting enough calcium and vitamin D:
- Adults under age 50 should have 1,000 mg of calcium and 400 to 800 International Units (IU) of vitamin D a day.
- Women ages 51 to 70 should have 1,200 mg of calcium and 400 to 800 IU of vitamin D a day.
- Men ages 51 to 70 should have 1,000 mg of calcium and 400 to 800 IU of vitamin D a day.
- Adults over age 70 should have 1,200 mg of calcium and 800 IU of vitamin D a day.
- Your provider may recommend a calcium supplement.
- Follow a diet that provides the proper amount of calcium and vitamin D. Use supplements to make up for the shortage only if your diet does not have the recommended amounts.
- Your provider may recommend higher doses of vitamin D if you have risk factors for osteoporosis or a low level of this vitamin.
(Note: Some expert groups are not sure the benefits and safety of these amounts of vitamin D and calcium outweigh their risks. Be sure to discuss with your provider whether supplements are a good choice for you.)
Stop unhealthy habits:
- Quit smoking, if you smoke.
- Limit your alcohol intake. Too much alcohol can damage your bones. This puts you at risk of falling and breaking a bone.
It is important to prevent falls by older people. These suggestions can help:
- Do not take medicines that make you drowsy and unsteady. If you must take them, be extra careful when you are up and moving around. For example, hold on to countertops or sturdy furniture to avoid falling.
- Remove household hazards, such as throw rugs, to reduce the risk of falls.
- Leave lights on at night so you can see better when walking around your house.
- Install and use safety grab bars in the bathroom.
- Install antislip flooring in bathtubs and showers.
- Make sure your vision is good. Have your eyes checked once or twice a year by an eye doctor.
- Wear shoes that fit well and have low heels. This includes slippers. Slippers that do not have heels can cause you to trip and fall.
- Do not walk outdoors alone on icy days.
Surgery to treat severe, disabling pain from spinal fractures due to osteoporosis include:
- Kyphoplasty (a material is placed into a bone of your spine to restore the height of the vertebrae)
- Spinal fusion (bones of your spine are joined together so they do not move against each other)
Outlook (Prognosis)
Medicines to treat osteoporosis can help prevent future fractures. Spine bones that have already collapsed can't be made stronger.
Osteoporosis can cause a person to become disabled from weakened bones. Hip fractures are one of the main reasons people are admitted to nursing homes.
Prevention
Be sure you get enough calcium and vitamin D to build and maintain healthy bones. Following a healthy, well-balanced diet can help you get these and other important nutrients.
Other tips for prevention:
- Do not drink large amounts of alcohol.
- Do not smoke.
- Get regular exercise.
Medicines can treat osteoporosis and prevent fractures. Your provider can tell you if any are right for you.
Related Information
MenopauseCushing syndrome
Hyperthyroidism
Hyperparathyroidism
Bulimia
Hip fracture surgery
Hip fracture - discharge
Preventing falls
References
Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393(10169):364-376. PMID: 30696576 pubmed.ncbi.nlm.nih.gov/30696576/.
De Paula FJA, Black DM, Rosen CJ. Osteoporosis: basic and clinical aspects. In: Melmed S, Auchus RJ, Goldfine AB, Loenig RJ, et al, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 30.
Eastell R, Rosen CJ, Black DM, et al. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society* clinical practice guideline. J Clin Endocrinol Metab. 2019;104(5):1595-1622. PMID: 30907593 pubmed.ncbi.nlm.nih.gov/30907953/.
Kemmler W, Bebenek M, Kohl M, von Stengel S. Exercise and fractures in postmenopausal women. Final results of the controlled Erlangen Fitness and Osteoporosis Prevention Study (EFOPS). Osteoporos Int. 2015;26(10):2491-2499. PMID: 25963237 pubmed.ncbi.nlm.nih.gov/25963237/.
LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Apr 28. Epub ahead of print. PMID: 35478046. pubmed.ncbi.nlm.nih.gov/35478046/.
Qaseem A, Forciea MA, McLean RM, et al. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839. PMID: 28492856 pubmed.ncbi.nlm.nih.gov/28492856/.
US Preventive Services Task Force, Grossman DC, Curry SJ, Owens DK, et al. Vitamin D, calcium, or combined supplementation for the primary prevention of fractures in community-dwelling adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(15):1592-1599. PMID: 29677309 pubmed.ncbi.nlm.nih.gov/29677309/.
BACK TO TOPReview Date: 1/16/2022
Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2022 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
