Polycystic kidney disease
Cysts - kidneys; Kidney - polycystic; Autosomal dominant polycystic kidney disease; ADPKD
Polycystic kidney disease (PKD) is a kidney disorder passed down through families. In this disease, many cysts form in the kidneys, causing them to become enlarged.
Causes
PKD is passed down through families (inherited). The two inherited forms of PKD are autosomal dominant and autosomal recessive.
People with PKD have many clusters of cysts in the kidneys. What exactly triggers the cysts to form is unknown.
PKD is associated with the following conditions:
- Aortic aneurysms
- Brain aneurysms
- Cysts in the liver, pancreas, and testes
- Diverticula of the colon
As many as half of people with PKD have cysts in the liver.
Symptoms
Symptoms of PKD may include any of the following:
- Abdominal pain or tenderness
- Blood in the urine
- Excessive urination at night
- Flank pain on one or both sides
- Drowsiness
- Joint pain
- Nail abnormalities
Exams and Tests
An examination may show:
- Abdominal tenderness over the liver
- Enlarged liver
- Heart murmurs or other signs of aortic insufficiency or mitral insufficiency
- High blood pressure
- Growths in the kidneys or abdomen
Tests that may be done include:
- Cerebral angiography
- Complete blood count (CBC) to check for anemia
- Liver tests (blood)
- Urinalysis
People with a personal or family history of PKD who have headaches should be tested to determine if cerebral aneurysms are the cause.
PKD and cysts on the liver or other organs may be found using the following tests:
If several members of your family have PKD, genetic tests can be done to determine whether you carry the PKD gene.
Treatment
The goal of treatment is to control symptoms and prevent complications. Treatment may include:
- Blood pressure medicines
- Diuretics (water pills)
- Low-salt diet
Any urinary tract infection should be treated quickly with antibiotics.
Cysts that are painful, infected, bleeding, or causing a blockage may need to be drained. There are usually too many cysts to make it practical to remove each cyst.
Surgery to remove one or both kidneys may be needed. Treatments for end-stage kidney disease may include dialysis or a kidney transplant.
Support Groups
More information and support for people with polycystic kidney disease and their families can be found at a kidney disease support group.
Outlook (Prognosis)
The disease gets worse slowly. Eventually, it may lead to end-stage kidney failure. It is also associated with liver disease, including infection of liver cysts.
Treatment may relieve symptoms for many years.
People with PKD who don't have other diseases may be good candidates for a kidney transplant.
Possible Complications
Health problems that may result from PKD include:
- Anemia
- Bleeding or rupture of cysts
- Long-term (chronic) kidney disease
- End-stage kidney disease
- High blood pressure
- Infection of liver cysts
- Kidney stones
- Liver failure (mild to severe)
- Repeated urinary tract infections
When to Contact a Medical Professional
Contact your health care provider if:
- You have symptoms of PKD
- You have a family history of PKD or related disorders and you are planning to have children (you may want to have genetic counseling)
Prevention
Currently, no treatment can prevent the cysts from forming or enlarging.
References
Arnaout MA. Cystic kidney diseases. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 118.
Torres VE, Harris PC. Cystic diseases of the kidney. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 45.
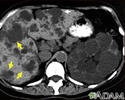
Kidney and liver cysts - CT scan - illustration
Kidney and liver cysts - CT scan
illustration
Liver and spleen cysts - CT scan - illustration
Liver and spleen cysts - CT scan
illustration
Review Date: 7/27/2021
Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.