Hypopituitarism
Pituitary insufficiency; Panhypopituitarism
Hypopituitarism is a condition in which the pituitary gland does not produce normal amounts of some or all of its hormones.
Causes
The pituitary gland is a small structure that is located just below the brain. It is attached by a stalk to the hypothalamus. The hypothalamus is the area of the brain that controls the pituitary gland's function.
The hormones released by the pituitary gland (and their functions) are:
- Adrenocorticotropic hormone (ACTH) -- stimulates the adrenal gland to release cortisol; cortisol helps to maintain blood pressure and blood sugar
- Antidiuretic hormone (ADH) -- controls water loss by the kidneys
- Follicle-stimulating hormone (FSH) -- controls sexual function and fertility in males and females
- Growth hormone (GH) -- stimulates growth of tissues and bone
- Luteinizing hormone (LH) -- controls sexual function and fertility in males and females
- Oxytocin -- stimulates the uterus to contract during labor and the breasts to release milk
- Prolactin -- stimulates female breast development and milk production
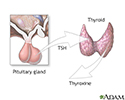
- Thyroid-stimulating hormone (TSH) -- stimulates the thyroid gland to release hormones that affect the body's metabolism
In hypopituitarism, there is a lack of one or more pituitary hormones. Lack of a hormone leads to loss of function in the gland or organ the hormone controls. For example, lack of TSH leads to loss of normal function of the thyroid gland.
Hypopituitarism may be caused by:
- Brain surgery
- Brain tumor
- Head trauma (traumatic brain injury)
- Infections or inflammation of the brain and the tissues that support the brain
- Death of an area of tissue in the pituitary gland (pituitary apoplexy)
- Radiation therapy to the brain
- Stroke (rare)
- Subarachnoid hemorrhage (from a burst aneurysm)
- Tumors of the pituitary gland or hypothalamus
Sometimes, hypopituitarism is due to uncommon immune system or metabolic diseases, such as:
- Too much iron in the body (hemochromatosis)
- Abnormal increase in immune cells called histiocytes (histiocytoses )
- Autoimmune condition that causes inflammation of the pituitary (lymphocytic hypophysitis)
- Inflammation of various tissues and organs (sarcoidosis)
- Infections of the pituitary, such as primary pituitary tuberculosis
Hypopituitarism is also a rare complication caused by severe bleeding during pregnancy. The loss of blood leads to tissue death in the pituitary gland. This condition is called Sheehan syndrome.
Certain medicines can also suppress pituitary function. The most common drugs are glucocorticoids (such as prednisone and dexamethasone), which are taken for inflammatory and immune conditions. Drugs used to treat prostate cancer can also lead to low pituitary function.
Symptoms
Symptoms of hypopituitarism include any of the following (multiple symptoms are common):
- Abdominal pain
- Decreased appetite
- Lack of sex drive (in men or women)
- Dizziness or fainting
- Excessive urination and thirst (including frequent urination at night)
- Failure to release milk (in women)
- Fatigue, weakness
- Headache
- Infertility (in women) or stopping of menstrual periods
- Loss of armpit or pubic hair
- Loss of the body or facial hair (in men)
- Low blood pressure
- Low blood sugar
- Sensitivity to cold
- Short height (less than 5 feet or 1.5 meters) if onset is during the childhood growth period
- Slowed growth and sexual development (in children)
- Vision problems
- Weight loss
Symptoms may develop slowly and may vary greatly, depending upon:
- The number of hormones that are missing and the organs they affect
- The severity of the disorder
Other symptoms that may occur with this disease:
Exams and Tests
To diagnose hypopituitarism, there must be low hormone levels due to a problem with the pituitary gland. The diagnosis must also rule out diseases of the organ that is affected by this hormone.
Tests may include:
- Brain CT scan
- Pituitary MRI
- ACTH
- Cortisol
- Estradiol (estrogen)
- Follicle-stimulating hormone (FSH)
- Insulin-like growth factor 1 (IGF-1)
- Luteinizing hormone (LH)
- Osmolality tests for blood and urine
- Testosterone level
- Thyroid-stimulating hormone (TSH)
- Thyroid hormone (T4)
- Biopsy of the pituitary
Level of a pituitary hormone may be high in the bloodstream if you have a pituitary tumor that is producing too much of that hormone. The tumor may crush other cells of the pituitary, leading to low levels of other hormones.
Treatment
If hypopituitarism is caused by a tumor, you may need surgery to remove the tumor. Radiation therapy may also be needed.
You will need lifelong hormone medicines to replace hormones that are no longer made by organs under the control of the pituitary gland. These may include:
- Corticosteroids (cortisol)
- Growth hormone
- Sex hormones (testosterone for men and estrogen for women)
- Thyroid hormone
- Desmopressin
Drugs are also available to treat related infertility in men and women.
If you take glucocorticoid medicines for pituitary ACTH deficiency, be sure you know when to take a stress dose of your medicine. Discuss this with your health care provider.
Always carry a medical ID (card, bracelet, or necklace) that says you have adrenal insufficiency. The ID should also say the type of medicine and dosage you need in case of an emergency caused by adrenal insufficiency.
Outlook (Prognosis)
Hypopituitarism is usually permanent. It requires lifelong treatment with one or more medicines. But you can expect a normal life span.
In children, hypopituitarism may improve if the tumor is removed during surgery.
Possible Complications
Side effects of medicines to treat hypopituitarism can develop. However, do not stop any medicine on your own without talking with your provider first.
When to Contact a Medical Professional
Call your provider if you develop symptoms of hypopituitarism.
Prevention
In most cases, the disorder is not preventable. Awareness of risk, such as from taking certain medicines, may allow early diagnosis and treatment.
References
Burt MG, Ho KKY. Hypopituitarism and growth hormone deficiency. In: Jameson JL, De Groot LJ, de Kretser DM, et al, eds. Endocrinology: Adult and Pediatric. 7th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 11.
Clemmons DR, Nieman LK. Approach to the patient with endocrine disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 208.
Fleseriu M, Hashim IA, Karavitaki N, et al. Hormonal replacement in hypopituitarism in adults: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(11):3888-3921. PMID: 27736313 pubmed.ncbi.nlm.nih.gov/27736313/.
Endocrine glands - illustration
Endocrine glands
illustration
The pituitary gland - illustration
The pituitary gland
illustration
Gonadotropins - illustration
Gonadotropins
illustration
Pituitary and TSH - illustration
Pituitary and TSH
illustration
Review Date: 5/13/2021
Reviewed By: Brent Wisse, MD, Board Certified in Metabolism/Endocrinology, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.