Health Library
Abdominal exploration
Exploratory surgery; Laparotomy; Exploratory laparotomy
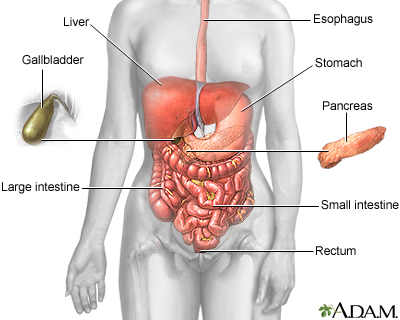
Abdominal exploration is surgery to look at the organs and structures in your belly area (abdomen). This includes your:
- Appendix
- Bladder
- Gallbladder
- Intestines
- Kidney and ureters
- Liver
- Pancreas
- Spleen
- Stomach
- Uterus, fallopian tubes, and ovaries (in women)
Surgery that opens the abdomen is called a laparotomy.
Images
Presentation

I Would Like to Learn About:
Description
Exploratory laparotomy is done while you are under general anesthesia. This means you are asleep and feel no pain.
The surgeon makes a cut into the abdomen and examines the abdominal organs. The size and location of the surgical cut depend on the specific health concern.
A biopsy can be taken during the procedure.
Laparoscopy describes a procedure that is performed with a tiny camera placed inside the abdomen. If possible, laparoscopy will be done instead of laparotomy.
Why the Procedure Is Performed
Your health care provider may recommend a laparotomy if imaging tests of the abdomen, such as x-rays and CT scans, have not provided an accurate diagnosis.
Exploratory laparotomy may be used to help diagnose and treat many health conditions, including:
- Cancer of the ovary, colon, pancreas, liver
- Endometriosis
- Gallstones
- Hole in the intestine (intestinal perforation)
- Acute appendicitis
- Diverticulitis
- Acute or chronic pancreatitis
- Liver abscess
- Pockets of infection (retroperitoneal abscess, abdominal abscess, pelvic abscess)
- Pregnancy outside of the uterus (ectopic pregnancy)
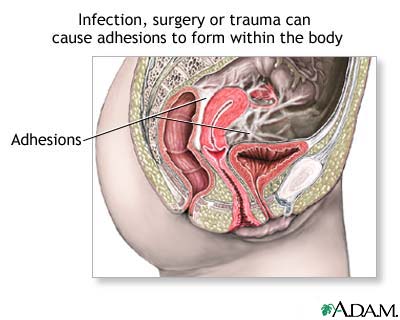
- Scar tissue in the abdomen (adhesions)
Risks
Risks of anesthesia and surgery in general include:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, infection
Risks of this surgery include:
- Incisional hernia
- Damage to organs in the abdomen
Before the Procedure
You will visit with your provider and have medical tests before your surgery. Your provider will:
- Do a complete physical exam.
- Make sure other medical conditions you may have, such as diabetes or high blood pressure, are under control.
- Perform tests to make sure that you will be able to tolerate the surgery.
- If you are a smoker, you should stop smoking several weeks before your surgery. Ask your provider for help.
Tell your provider:
- What prescription and over-the-counter medicines you are taking
- Any vitamins, herbs, and other supplements you are taking
- If you have been drinking a lot of alcohol, more than 1 or 2 drinks a day
- If you might be pregnant
During the week before your surgery:
You may be asked to temporarily stop taking blood thinners. Some of these are:
- Aspirin
- Ibuprofen (Advil, Motrin)
- Vitamin E
- Warfarin (Coumadin)
- Clopidogrel (Plavix)
- Ticlopidine (Ticlid)
Ask your provider which drugs you should still take on the day of your surgery.
Prepare your home for your return from the hospital.
On the day of your surgery:
- Follow your provider's instructions about when to stop eating and drinking.
- Take medicines your provider told you to take with a small sip of water.
- Arrive at the hospital on time.
Outlook (Prognosis)
You should be able to start eating and drinking normally about 2 to 3 days after the surgery. How long you stay in the hospital depends on the severity of the problem. Complete recovery usually takes about 4 to 6 weeks.
Related Information
X-rayCT scan
Biopsy
Appendicitis
Acute
Chronic pancreatitis
Peritonitis - spontaneous bacterial
Endometriosis
Pelvic inflammatory disease (PID)
Adhesion
Cancer
Diverticulitis
Ectopic pregnancy
Hodgkin lymphoma
References
Landmann A, Bonds M, Postier R. Acute abdomen. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 46.
Sham JG, Reames BN, He J. Management of periampullary cancer. In: Cameron AM, Cameron JL, eds. Current Surgical Therapy. 13th ed. Philadelphia, PA: Elsevier; 2020:545-552.
BACK TO TOPReview Date: 2/28/2022
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2022 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
