Health Library
Pancreatic pseudocyst
Pancreatitis - pseudocyst
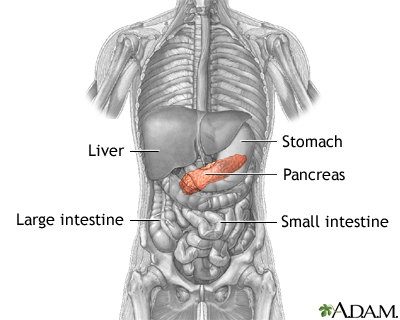
A pancreatic pseudocyst is a fluid-filled sac in the abdomen that arises from the pancreas. It may also contain tissue from the pancreas, enzymes, and blood.
Images
I Would Like to Learn About:
Causes
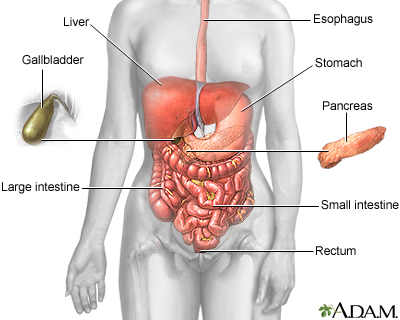
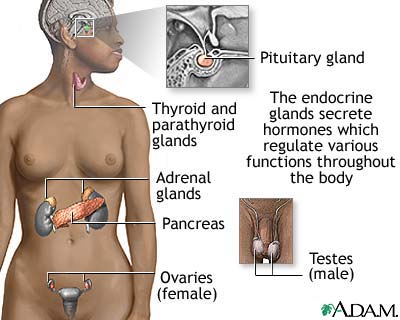
The pancreas is an organ located behind the stomach. It produces chemicals (called enzymes) needed to digest food. It also produces the hormones insulin and glucagon.
Pancreatic pseudocysts most often develop after an episode of severe pancreatitis. Pancreatitis happens when your pancreas gets inflamed. There are many causes of this problem.
This problem may sometimes occur:
- In someone with long-term (chronic) swelling of the pancreas (pancreatitis), most often due to alcohol abuse
- After trauma to the belly, more often in children
The pseudocyst happens when the ducts (tubes) in the pancreas are damaged and fluid with enzymes cannot drain.
Symptoms
Symptoms can occur within days to months after an attack of pancreatitis. They include:
- Bloating of the abdomen
- Constant pain or deep ache in the abdomen, which may also be felt in the back
- Nausea and vomiting
- Loss of appetite
- Difficulty eating and digesting food
Exams and Tests
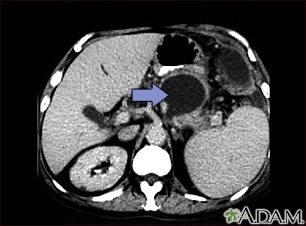
The health care provider may feel your abdomen for a pseudocyst. It will feel like a lump in the middle or left upper abdomen.
Tests that may help detect pancreatic pseudocyst include:
- Abdominal CT scan
- Abdominal MRI
- Abdominal ultrasound
- Endoscopic ultrasound (EUS)
Treatment
Treatment depends on the size of the pseudocyst and whether it is causing symptoms. Many pseudocysts go away on their own. Those that remain for more than 6 weeks and are larger than 5 centimeters (about 2 inches) in diameter often need treatment.
Possible treatments include:
- Drainage through the skin using a needle, most often guided by a CT scan.
- Endoscopic-assisted drainage using an endoscope. In this, a tube containing a camera and a light is passed down into the stomach)
- Surgical drainage of the pseudocyst. A connection is made between the cyst and the stomach or small intestine. This may be done using a laparoscope.
Outlook (Prognosis)
The outcome is generally good with treatment. It is important to make sure that it is not a pancreatic cancer that starts in a cyst, which has a worse outcome.
Possible Complications
Complications may include:
- A pancreatic abscess can develop if the pseudocyst becomes infected.
- The pseudocyst can break open (rupture). This can be a serious complication because shock and excess bleeding (hemorrhage) may develop.
- The pseudocyst may press down on (compress) nearby organs.
When to Contact a Medical Professional
If you are known to have a pseudocyst, rupture of the pseudocyst is a medical emergency. Go to the emergency room or call the local emergency number (such as 911) if you develop symptoms of bleeding or shock, such as:
- Fainting
- Fever and chills
- Rapid heartbeat
- Severe abdominal pain
Prevention
The way to prevent pancreatic pseudocysts is by preventing pancreatitis. If pancreatitis is caused by gallstones, the provider will perform surgery to remove the gallbladder (cholecystectomy).
When pancreatitis occurs due to alcohol abuse, you must stop drinking alcohol to prevent future attacks.
When pancreatitis occurs due to high blood triglycerides, this condition should be treated.
Related Information
Acute pancreatitisChronic pancreatitis
Shock
Pancreatic abscess
References
Forsmark CE. Pancreatitis. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 135.
Martin MJ, Brown CVR. Management of pancreatic pseudocyst. In: Cameron AM, Cameron JL, eds. Current Surgical Therapy. 13th ed. Philadelphia, PA: Elsevier; 2020:525-536.
Vege SS. Acute pancreatitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 58.
BACK TO TOPReview Date: 10/25/2021
Reviewed By: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2022 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
