Endocardial cushion defect
Atrioventricular (AV) canal defect; Atrioventricular septal defect; AVSD; Common AV orifice; Ostium primum atrial septal defects; Congenital heart defect - ECD; Birth defect - ECD; Cyanotic disease - ECD
Endocardial cushion defect (ECD) is an abnormal heart condition. The walls separating all four chambers of the heart are poorly formed or absent. Also, the valves separating the upper and lower chambers of the heart have defects during formation. ECD is a congenital heart disease, which means it is present from birth.
Causes
ECD occurs while a baby is still growing in the womb. The endocardial cushions are two thicker areas that develop into the walls (septum) that divide the four chambers of the heart. They also form the mitral and tricuspid valves. These are the valves that separate the atria (top collecting chambers) from the ventricles (bottom pumping chambers).
The lack of separation between the two sides of the heart causes several problems:
- Increased blood flow to the lungs. This results in increased pressure in the lungs. In ECD, blood flows through the abnormal openings from the left to the right side of the heart, then to the lungs. More blood flow into the lungs makes the blood pressure in the lungs rise.
- Heart failure. The extra effort needed to pump makes the heart work harder than normal. The heart muscle may enlarge and weaken. This can cause swelling in the baby, problems in breathing, and difficulty in feeding and growing.
- Cyanosis. As the blood pressure increases in the lungs, blood starts to flow from the right side of the heart to the left. The oxygen-poor blood mixes with the oxygen-rich blood. As a result, blood with less oxygen than usual is pumped out to the body. This causes cyanosis, or bluish skin.
There are two types of ECD:
- Complete ECD. This condition involves an atrial septal defect (ASD) and a ventricular septal defect (VSD). People with a complete ECD have only one large heart valve (common AV valve) instead of two distinct valves (mitral and tricuspid).
- Partial (or incomplete) ECD. In this condition, only an ASD, or an ASD and VSD are present. There are two distinct valves, but one of them (the mitral valve) is often abnormal with an opening ("cleft") in it. This defect can leak blood back through the valve.
ECD is strongly linked to Down syndrome. Several gene changes are also linked to ECD. However, the exact cause of ECD is unknown.
ECD may be associated with other congenital heart defects, such as:
Symptoms
Symptoms of ECD may include:
- Baby tires easily
- Bluish skin color, also known as cyanosis (the lips may also be blue)
- Feeding difficulties
- Failure to gain weight and grow
- Frequent pneumonia or infections
- Pale skin (pallor)
- Rapid breathing
- Rapid heartbeat
- Sweating
- Swollen legs or abdomen (rare in children)
- Trouble breathing, especially during feeding
Exams and Tests
During an exam, the health care provider will likely find signs of ECD, including:
- An abnormal electrocardiogram (ECG)
- An enlarged heart
- Heart murmur
Children with partial ECD may not have signs or symptoms of the disorder during childhood.
Tests to diagnose ECD include:
- Echocardiogram, which is an ultrasound that views the heart structures and blood flow inside the heart
- ECG, which measures the electrical activity of the heart
- Chest x-ray
- MRI, which provides a detailed image of the heart
- Cardiac catheterization, a procedure in which a thin tube (catheter) is placed into the heart to see blood flow and take accurate measurements of blood pressure and oxygen levels
Treatment
Surgery is needed to close the holes between the heart chambers, and to create distinct tricuspid and mitral valves. The timing of the surgery depends on the child's condition and the severity of the ECD. It can often be done when the baby is 3 to 6 months old. Correcting an ECD may require more than one surgery.
Your child’s doctor may prescribe medicine:
- To treat the symptoms of heart failure
- Before surgery if ECD has made your baby very sick
The medicines will help your child gain weight and strength before surgery. Medicines often used include:
- Diuretics (water pills)
- Drugs that make the heart contract more forcefully (inotropic agents)
Surgery for a complete ECD should be done in the baby's first year of life. Otherwise, lung damage that may not be able to be reversed can occur. Babies with Down syndrome tend to develop lung disease earlier. Therefore, early surgery is very important for these babies.
Outlook (Prognosis)
How well your baby does depends on:
- The severity of the ECD
- The child's overall health
- Whether lung disease has already developed
Many children live normal, active lives after ECD is corrected.
Possible Complications
Complications from ECD may include:
- Congestive heart failure
- Death
- Eisenmenger syndrome
- High blood pressure in the lungs
- Irreversible damage to the lungs
Certain complications of ECD surgery may not appear until the child is an adult. These include heart rhythm problems and a leaky mitral valve.
Children with ECD may be at risk for infection of the heart (endocarditis) before and after surgery. Ask your child's doctor whether your child needs to take antibiotics before certain dental procedures.
When to Contact a Medical Professional
Contact your child's provider if your child:
- Tires easily
- Has trouble breathing
- Has bluish skin or lips
Also talk to the provider if your baby is not growing or gaining weight.
Prevention
ECD is linked to several genetic abnormalities. Couples with a family history of ECD may wish to seek genetic counseling before becoming pregnant.
References
Basu SK, Dobrolet NC. Congenital defects of the cardiovascular system. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 75.
Ebels T, Tretter JT, Spicer DE, Anderson RH. Antroventricular septal defects. In: Wernovsky G, Anderson RH, Kumar K, et al. Anderson's Pediatric Cardiology. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 31.
Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM. Acyanotic congenital heart disease: left-to-right shunt lesions. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 453.
Congenital heart defects (CHD) overview
Animation
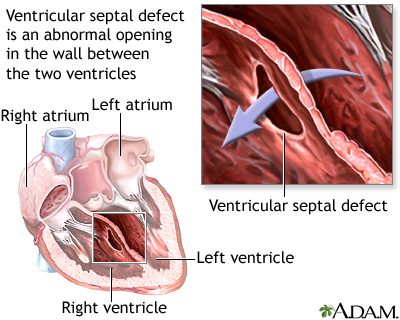
Ventricular septal defect - illustration
Ventricular septal defect
illustration
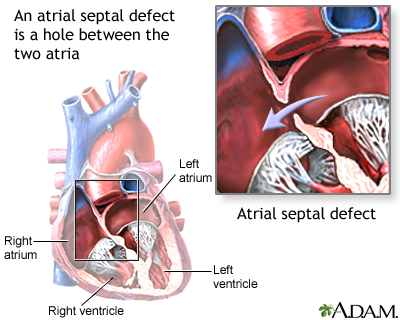
Atrial septal defect - illustration
Atrial septal defect
illustration
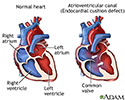
Atrioventricular canal (endocardial cushion defect) - illustration
Atrioventricular canal (endocardial cushion defect)
illustration
Review Date: 5/8/2022
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.